What you need to know about diabetic peripheral neuropathy
Diabetic peripheral neuropathy is a type of nerve damage that affects approximately 10 million Americans. While it can be painful, the condition is manageable if the damage is properly diagnosed and treated by medical professionals. If you or a loved one is living with diabetic neuropathy, educating yourself is an important first step.
What is peripheral neuropathy?
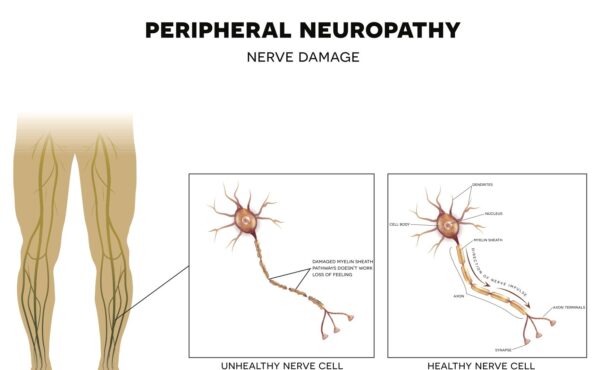
Peripheral neuropathy — one of four primary types of diabetic neuropathy — is a condition caused by damage to one or more of the nerves that live outside of the brain and spinal cord. Collectively referred to as the peripheral nervous system, these nerves provide us with the ability to move, sense the world around us, and regulate vital functions such as heart rate, blood pressure and digestion.
While damage to peripheral nerves can occur anywhere, it is typically first experienced in the toes and fingers. As the damage progresses, individuals with this type of peripheral neuropathy will frequently experience a spread of symptoms that is referred to as a “stocking and glove” pattern, in which the entire foot and/or hand becomes affected.
What causes peripheral neuropathy?
Peripheral neuropathy can be caused by a variety of medical conditions, including autoimmune diseases, such as rheumatoid arthritis and lupus, and certain drugs used in the treatment of cancer. Alcohol abuse, vitamin deficiencies, infections, and exposures to toxins, such as lead and mercury, have also been shown to cause neuropathy. However, the most common cause of peripheral neuropathy is diabetes.
In diabetic patients, peripheral nerve damage is thought to be caused by long-term exposure to elevated blood sugar levels. High blood sugars are believed to cause direct damage to nerve fibers and impair their ability to transmit signals to the brain. Increased blood sugars have also been shown to cause damage to the blood vessels that supply the oxygen and nutrition needed for nerve fibers to function properly. Additionally, higher levels of a type of fat called triglycerides have been linked to an increased risk for the development of peripheral neuropathy in a variety of conditions including diabetes.
Peripheral neuropathy is the most common complication of diabetes and is present in almost 10% of patients by the time their diabetes is diagnosed. Studies have shown that up to 50% of all diabetics will eventually experience some form of neuropathy.
What are the symptoms of peripheral neuropathy?
Symptoms of peripheral neuropathy vary, but typically include pain — often described as a burning or electric-shock-like sensation — as well as numbness and tingling. People may also experience a sensation called allodynia, in which pain is felt in response to stimulations that are typically not painful, such as a light touch or the feel of clothing.
Other symptoms can include:
- Muscle weakness and balance issues due to the inability to feel where the feet are while standing or walking
- Excessive sweating or heat intolerance caused by abnormal sweat gland function
- Nausea, vomiting, and bloating due to impaired digestion
- Dizziness or fainting when arising from a lying or sitting position as the result of changes in blood pressure
What are risk factors for diabetic neuropathy?
The leading risk factor for neuropathy — and all complications caused by diabetes — is poor control over blood sugar levels. Kidney damage due to poorly controlled diabetes increases the risk for neuropathy due to the presence of elevated levels of toxins in the blood. Almost 90% of diabetics are either overweight or obese, while more than 40% have elevated triglyceride and cholesterol levels — both of which have been shown to increase the risk for diabetic neuropathy. Smoking also increases risk by reducing the flow of blood, oxygen, and nutrients to the nerves in the hands and feet.
It is important to note that while many diabetics will experience neuropathy, addressing the above risk factors can not only decrease the chance of its occurrence, but also reduce the risk for worsening once neuropathy has occurred.
How is diabetic neuropathy diagnosed?
The diagnosis of diabetic neuropathy begins with a comprehensive neurological examination. Other basic assessments include muscle strength testing, as well as reflexes and sensory examinations. Patients are assessed based on their ability to feel light touch, pin prick, vibration, pressure, temperature, and changes in position.
More advanced testing may be considered when the exact cause of the neuropathy is unclear or when additional information is needed to guide treatment. Electrodiagnostic testing is used to evaluate the speed of nerve signaling and how muscles respond to those signals in order to identify the severity and location of nerve damage. Gastric emptying tests are performed when a patient with diabetes experiences problems with digestion. Similarly, autonomic testing to examine changes in blood pressure and sweating is performed when damage to the nerves controlling cardiovascular and endocrine system functions is suspected. Skin biopsies can also be useful in determining the severity of nerve damage.
Join a diabetic neuropathy clinical trial
Are you living with diabetic peripheral neuropathy? Consider advancing treatment options for yourself and other patients around the world by joining a clinical trial. MedVadis Research is currently recruiting participants for a clinical research study that evaluates an investigational product for diabetic peripheral neuropathic pain. Learn morehere
Ready to Participate?
Take a look at our current trials or join our mailing list to find the right study for you.
Together, we can advance medical treatments for generations.

What is a memory screening?
If you are not worried about your memory, you may not have considered participating in a memory screening.

Q&A with Dr. Egilius L.H. Spierings
Dr. Egilius L.H. Spierings founded MedVadis Research—then known as the Clinical Headache Research Center—in 1994. Having dedicated the last four decades…

Diabetic neuropathy: Current treatment options & clinical research
Diabetic neuropathy—or nerve damage—is a common and serious complication of diabetes.
